Combined Oral Contraceptive Treatment Does Not Alter the Gut Microbiome or Serum Metabolomic Profile in Obese Girls with Polycystic Ovary Syndrome
Beza Jobira1,2, Daniel N. Frank2, Lori J. Silveir3, Yesenia Garcia-Reyes1, Charles E. Robertson2, Diana Ir2, Keisha L Alexander5, Angelo D’Alessandro6, Kristen J. Nadeau1,4, and Melanie Cree-Green1,4
1Department of Pediatrics, Division of Pediatric Endocrinology, University of Colorado, Anschutz Medical Campus, Aurora, CO; 2Department of Medicine, Division of Infectious Diseases, University of Colorado Anschutz, Medical Campus, Aurora, CO; 3Department of Biostatistics and Informatics, Colorado School of Public Health, Aurora, CO; 4Center for Women’s Health Research, University of Colorado Anschutz Medical Campus, Aurora, CO; 5University of Colorado Anschutz Medical Campus Pharmaceutical Science, Aurora, CO; 6University of Colorado Anschutz medical Campus School of Medicine, Biochemistry and Molecular Genetics, Aurora, CO
Background: The gut microbiome is altered in obese adolescents with polycystic ovary syndrome (PCOS), and is associated with free testosterone, metabolic markers and insulin resistance. Combined oral contraceptives (OCP) are a primary treatment for PCOS and lower testosterone, but it was unknown if they changed the gut microbiome in obese adolescents with PCOS. Objective: Assess the gut microbiome profile, targeted serum metabolomics, hormonal and metabolic measures in adolescents with PCOS and obesity with and without OCP treatment. Methods: Adolescent girls with PCOS and obesity, with and without OCP treatment, were recruited from a tertiary referral hospital and underwent stool and fasting blood collection, an oral glucose tolerance test and MRI for hepatic fat fraction. Fecal bacterial were profiled by high throughput 16S rRNA gene sequencing and fasting serum metabolomics performed with mass spectroscopy. Groups were compared with t-tests and correlations performed. Results: Twenty-nine obese adolescents with PCOS [Untreated N=21, 16±1.2 years, BMI%ile 36.5± 3.0; OCP N=8, 15.5±0.9, BMI%ile 32.5±3.9] participated. OCP therapy had lower free testosterone and higher SHBG (p<0.001). Platelets were significantly higher (p=0.01), along with a trend in elevated CRP (p=0.09) in the OCP group. There was no difference in measures of fasting glucose, insulin or lipids. Measures of insulin resistance including HOMA-IR and Matsuda were also similar. Principle components analysis of the serum metabolome was not different between the groups. Girls treated with OCP had similar stool microbiome α-diversity measures of bacterial evenness (p=0.28), bacterial diversity (p=0.15), and global microbial composition (b-diversity, p=0.56). Further, the percent relative abundance (%RA) of the Firmicutes: Bacteroidetes ratio was similar, as well as the %RA at the phyla, family and genus level. Bacterial a-diversity was negatively associated with serum bile acids and branched chain amino acids. A higher %RA of family Ruminococcaceae was significantly associated with serum conjugated bile acids and HOMA-IR. Conclusion: Despite changes in free testosterone and SHBG, adolescent girls with PCOS treated with OCP had similar clinical and gut microbiome profile compared to the untreated PCOS group. The significant association between bacterial a-diversity, Ruminococcaceae, clinical markers and bile acids suggests a potential role of the gut microbiome in the pathogenesis of metabolic syndrome and PCOS.
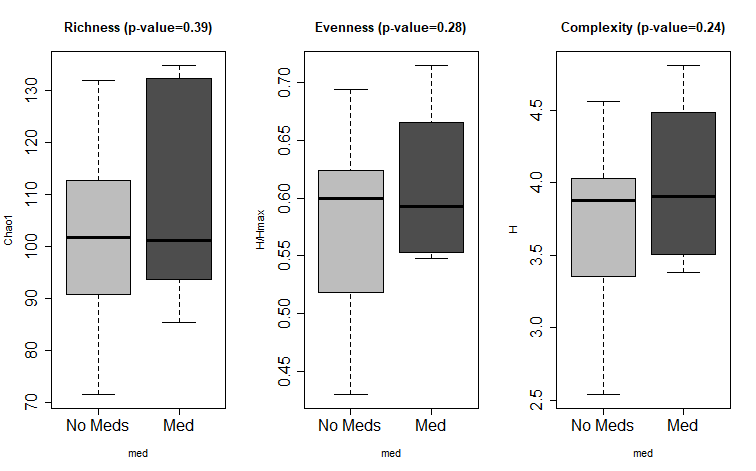 |
Figure 1: Alpha biodiversity measures. Measures of α-biodiversity including Richness (Chao1); Evenness (H/Hmax), and Diversity (H). There were no statistical differences in α-diversity between groups. |
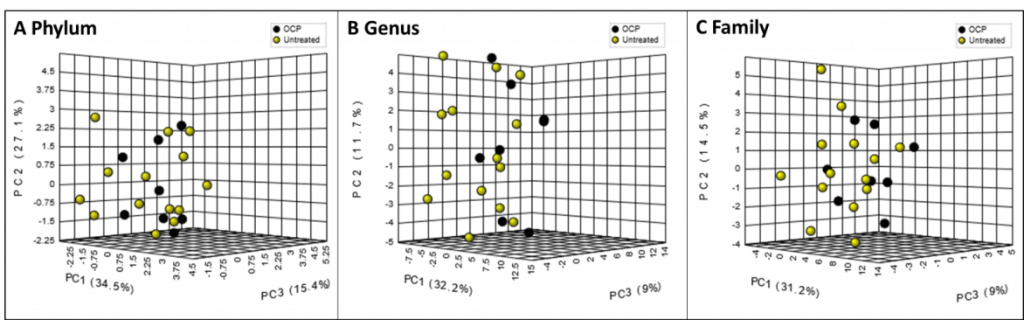 |
Figure 2: Percent relative abundance (%RA) in OCP treatment and no treatment group. Principal component analysis of bacterial %RA between groups at the A) Phyla, B) Genus, C) Family levels. There were no statistical difference in %RA between groups. |
Breakout Room: Jobira, Beza
View Poster: https://uclacns.org/symposium2021/12-Jobira-Beza.pdf
