A Distinct Brain-Gut-Microbiome Profile Exists for Females with Obesity and Food Addiction
Tien S. Dong1-3,5, Emeran A. Mayer1-5, Vadim Osadchiy,4,5 Candace Chang3, William Katzka3, Venu Lagishetty1,3,5, Kimberly Gonzalez1,4,5, Amir Kalani1,5, Jean Stains1,4,5, Jonathan P. Jacobs1-6, Valter D. Longo7, Arpana Gupta1-5
1Vatche and Tamar Manoukian Division of Digestive Diseases, 2David Geffen School of Medicine, 3UCLA Microbiome Center, 4G. Oppenheimer Center for Neurobiology of Stress and Resilience, 5University of California, Los Angeles, 6Division of Gastroenterology, Hepatology and Parenteral Nutrition, VA Greater Los Angeles Healthcare System, Los Angeles, CA,7USC Longevity Institute, University of Southern California, Los Angeles
Background: Obesity and its comorbidities represent a major global health problem. It has been suggested that food addiction, especially to highly processed foods, may contribute to this rising epidemic. Alterations in brain-gut-microbiome interactions have been implicated as an important factor in eating behaviors and in the development of obesity. We aimed to explore a novel relationship between food addiction and the brain-gut-microbiome axis using a multi’omics approach involving 16S rRNA sequencing, metabolomics, and brain imaging in females with high BMIs. lterations in brain-gut-microbiome interactions have been implicated as an important factor in obesity. We aimed to explore the relationship between food addiction (FA) and the brain-gut-microbiome axis using a multi’omics approach involving microbiome data, metabolomics, and brain imaging. Methods: Structural and diffusion tensor magnetic resonance imaging was obtained in 105 females with high BMIs (³25kg/m2). The Yale Food Addiction Scale (YFAS) was administered and food addiction was defined as a score >3. Fecal samples were collected for 16S sequencing and metabolomics. Multivariate analyses were used to determine the relationship between food addiction with 16S rRNA profiles, metabolomics data, and brain anatomical connectivity measures. Results: The average age was 32.4 years+10.1 with an average BMI of 30.3+5.9. Of the females with obesity, 33% (17/51) exhibited food addiction behavior as per YFAS score compared to 15.8% (6/38) and 0% (0/16) (p=0.0001). Based on a multilevel sparse partial least square discriminant analysis, there was a difference in the gut microbiome of females with FA versus those without. Differential abundance testing showed Bacteroides, Megamonas, Eubacterium and Akkermansia were statistically associated with FA (q-value<0.05). There were no differences in species richness, evenness, or diversity between those with food addiction versus those without. Metabolomics showed that indolepropionic acid was inversely correlated to FA. FA was also correlated with increased connectivity within the brain’s reward network, specifically between the intraparietal sulcus, brain stem and putamen. Conclusion: The finding supports our hypothesis that alterations at different levels of the brain-gut-microbiome axis are involved in abnormal eating behaviors and obesity in females. Even though cross-sectional, the results provide important information for future mechanistic studies.
| Table 1: Baseline Characteristics by Food Addiction | SD: Standard deviation | |||
| No Food Addiction (No FA) (n=86) | Food Addiction (FA) (n=19) | p-value | ||
| Age (mean +/- SD) (yrs) | 33.19 + 10.31 | 28.57 + 8.66 | 0.07 | |
| BMI (mean +/- SD) | 29.1 + 5.4 | 35.6+ 5.3 | 0.0001 | |
| Normal Weight (n=16) % | 18.60 | 0.00 | 0.0001 | |
| Overweight (n=38) % | 41.86 | 10.52 | ||
| Obese (n=51) % | 39.53 | 89.47 | ||
| YFAS Symptom Count (mean +/- SD) | 1.15 + 0.77 | 3.63 + 1.16 | <0.0001 | |
| Race/Ethnicity | ||||
| Hispanic (n=41) % | 36.05 | 52.63 | 0.55 | |
| Caucasian (n=28) % | 23.26 | 42.11 | ||
| African American (n=13) % | 12.79 | 10.53 | ||
| Asian (n=21) % | 20.93 | 15.79 | ||
| Other (n=2) % | 2.33 | 0 | ||
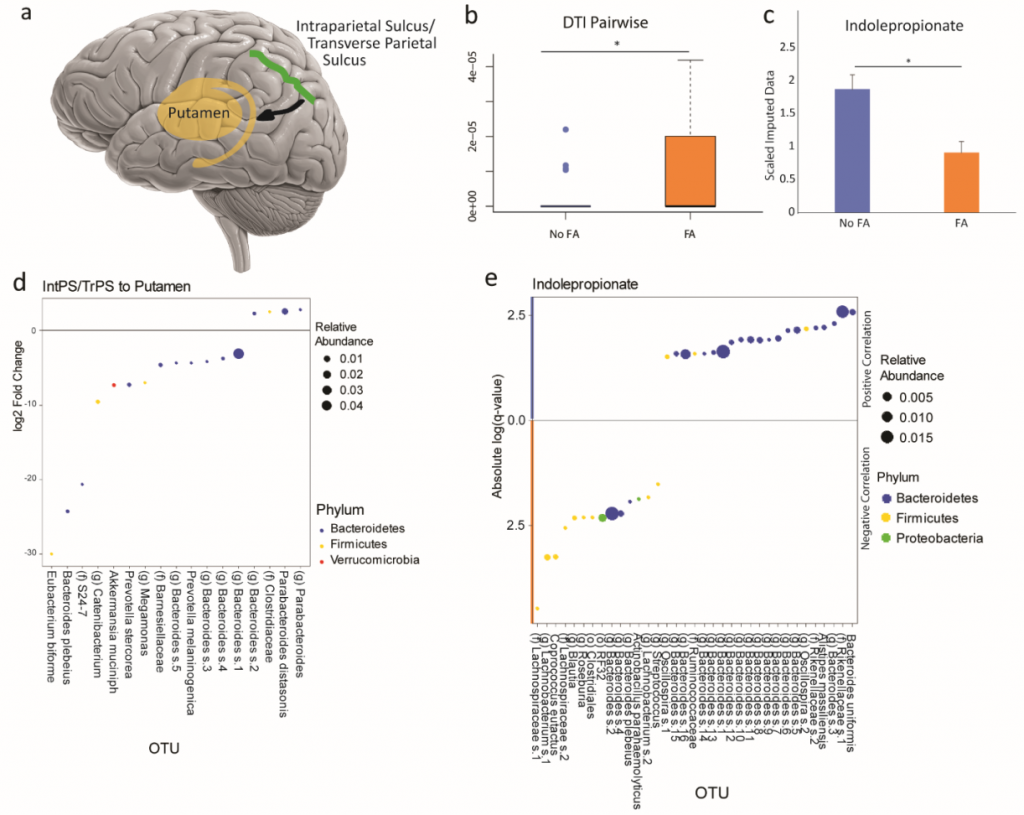 |
Figure 1: Brain imaging and Indolepropionate is associated with food addiction. DTI pairwise showed that the communication between the intraparietal sulcus/transverse parietal (IntPS/TrPS) sulcus and brain stem to the putamen was positively associated with Food Addiction (FA) in patients with obesity. A) Schematic diagram of the significant brain region associated with food addiction and its quantification (B and C). D) Levels of fecal indolepropionate in obese subjects with or without food addiction (FA). E) DESEq2 analysis in obese subjects showing several OTUs associated with increase connectivity between the brain stem and the putamen. F) DESEq2 analysis in obese subjects showing several OTUs associated with increase connectivity between the IntPS/TrPS to the putamen. G) The OTUs that are correlated to fecal indolepropionate by DESEq2 in patients with obesity. IntPS/TrPS: intraparietal sulcus/transverse parietal sulcus. Pu: Putamen. |
Breakout Room: Dong, Tien
View Poster: https://uclacns.org/symposium2021/10-Dong-Tien.pdf
